What is Ankylosing Spondylitis
Ankylosing Spondylitis (AS) is a chronic inflammatory arthritis primarily affecting the spine and sacroiliac joints, leading to pain, stiffness, and loss of mobility. This condition falls under the broader category of spondyloarthritis, which encompasses a group of inflammatory diseases targeting the spine and peripheral joints.
Key characteristics of Ankylosing Spondylitis include:
- Inflammatory Back Pain: AS typically begins with insidious onset inflammatory back pain, involving the lower back and buttocks. The pain is often worse in the morning or after periods of inactivity and may improve with exercise.
- Sacroiliitis: Inflammation of the sacroiliac joints, which connect the spine to the pelvis, is a hallmark feature of AS. This can contribute to lower back pain and stiffness.
- Spinal Fusion: Over time, chronic inflammation in the spine can lead to the formation of new bone, causing vertebrae to fuse together. This process, called ankylosis, can result in a rigid and less flexible spine.
- Peripheral Joint Involvement: While the spine is predominantly affected, AS can also impact other joints, including the hips, knees, and shoulders.
- Enthesitis: Inflammation at the sites where tendons and ligaments attach to bones, known as entheses, is common in AS. This can lead to pain and swelling in areas such as the heels and bottom of the feet.
- Systemic Manifestations: Ankylosing Spondylitis is not limited to the musculoskeletal system. It can involve other organs and systems, leading to conditions such as uveitis (inflammation of the eye), Inflammatory Bowel Disease (IBD), skin disorders like Psoriasis, and, in rare cases, cardiovascular or respiratory complications.
- Onset and Diagnosis: AS often starts in early adulthood, with males more commonly affected than females. Diagnosis involves a combination of clinical symptoms, imaging studies (such as X-rays and MRI), and blood tests.
Ankylosing Spondylitis Symptoms
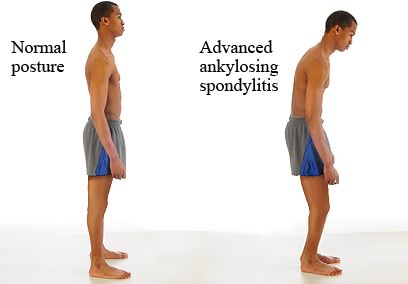
The early symptom of this disease is morning stiffness, which is basically, when the patient gets up in the morning there is stiffness in the lower back. Sometimes, the pain disturbs the sleep pattern as it occurs at say 4 in the morning. The stiffness disappears once they start walking in the morning. This happens in the beginning but as the disease progresses, patient’s posture becomes stooped due to the deformity in the patient’s spine. This is reflected when the patient bends forward. Over time, the hips become stiff and later on even the neck become stiff. It’s a very disabling disease for a young man.
Impact of Ankylosing Spondylitis on patient body
As Ankylosing Spondylitis (AS) progresses over several years, its impact extends beyond the initial lower back pain, advancing towards the waist and influencing the patient's posture.
Prolonged suffering often leads to reduced activity levels, exacerbating the challenges faced by individuals with AS.
Beyond the primary symptoms of back pain, AS can manifest in major joints, particularly in individuals diagnosed at a younger age. The involvement of peripheral joints sometimes necessitates surgical interventions. Reduced physical activity contributes to muscular weakness, further complicating the overall health of the patient.
The initial localized pain evolves into widespread body aches, significantly affecting the quality of life for AS patients. A distinctive ocular manifestation, known as uveitis, can occur, causing sensitivity to light and impairing visual acuity. Additionally, AS patients may develop Inflammatory Bowel Disease (IBD), experience skin complications such as Psoriasis, and contend with anemia and associated weakness.
In rare instances, AS can impact vital organs such as the heart, lungs, and kidneys, underscoring the systemic nature of the disease. The multifaceted challenges posed by AS necessitate a comprehensive approach to management, involving not only musculoskeletal care but also considerations for ocular, gastrointestinal, dermatological, and hematological aspects. Increased awareness of these diverse manifestations is essential for a holistic understanding of the impact of Ankylosing Spondylitis on patients' overall well-being.
Reasons behind Pain in Ankylosing
It is imperative to be aware of potential serious complications associated with Ankylosing Spondylitis (AS), even though they are rare. Particularly, understanding the transformation of the spine into a condition known as "bamboo spine" is crucial. In the normal physiological state, the spine exhibits a high degree of flexibility. However, in individuals with AS, calcification alters the spine's structure, rendering it rigid and brittle, akin to delicate china bone crockery. This transformation results in the fusion of the individual vertebrae into a single, inflexible structure, eliminating the natural flexibility of the spine found in unaffected individuals.
The heightened fragility of the spine in individuals with AS poses a significant risk. Even minor incidents or injuries can lead to spine fractures, with a proclivity for occurrences near the neck area. It is essential to note that in a normal spine, comprised of a chain of 30–32 bones, fractures are less likely due to the distributed flexibility across multiple vertebrae. However, in the context of AS-induced calcification and fusion, the spine essentially becomes a singular, unyielding bone structure, magnifying the vulnerability to fractures.
Detecting these fractures presents a considerable challenge. The extensive calcification throughout the spine results in X-ray imaging portraying the entire spine uniformly in white, obscuring potential fracture lines. This complicates the diagnostic process and underscores the importance of heightened vigilance and specialized imaging techniques in identifying fractures promptly.
Families with individuals affected by AS should be cognizant of these potential complications, emphasizing the need for proactive monitoring, timely medical intervention, and a collaborative approach between patients, their families, and healthcare providers to manage and mitigate such risks.
How to overcome the Ankylosing
Individuals with longstanding spinal deformity due to conditions like Ankylosing Spondylitis (AS) often exhibit a forward-bent posture. Notably, if such patients experience a sudden correction in their deformity after an impact or hit, it could signify an underlying spinal fracture. Any instance where a patient reports persistent pain warrants thorough investigation, as continuous pain, especially after a period of relative relief, raises concerns about potential fractures.
The active phase of AS is initially characterized by painful symptoms, which tend to subside over the years as bone fusion occurs. However, the sudden onset of pain should prompt an evaluation for possible fractures. Diagnostic tools such as CT scans or MRI of the spine become essential in ruling out fractures, especially when dealing with the cervical region. In patients with AS, the Altanto-Axial joint, crucial for head movement, can become unstable, posing a risk of dislocation during sudden movements. This dislocation requires urgent attention to prevent severe consequences, including paralysis or even fatality.
Surgical interventions for fractures in these patients necessitate special considerations, particularly during general anesthesia administration. The Altanto-Axial joint's instability requires a specialized flexible tube insertion, given the restricted neck movement in these individuals. Attendants and medical professionals must exercise caution in handling AS patients during transport and medical procedures to avert potential complications, especially if the treating healthcare providers are unfamiliar with the patient's underlying condition.
Informing healthcare providers about the patient's AS during emergencies is critical, as the absence of visible deformities might lead to mismanagement. Proper communication aids in ensuring that medical professionals comprehend the unique challenges associated with AS, preventing inadvertent harm during interventions.
Furthermore, individuals with AS often present with diminished chest expansion, leading to compromised lung function. As they age, susceptibility to chest infections increases. Initiating treatment promptly after an infection is paramount, given their limited lung capacity. This proactive approach is essential in managing respiratory health and minimizing complications associated with pulmonary issues in individuals with Ankylosing Spondylitis.
Looking for Best Ankylosing Spondylitis Doctor in Delhi? Contact Dr. Ashwani Maichand today.
Our Services

Dr. Ashwani Maichand
MBBS, MS(Orthopaedics) | Mch(Orthopaedics)
- Sr. Consultant & Director at Minomax Orthopaedics
- Director Orthopaedics, CK Birla Hospital
- Fellowship Joint Replacement (USA & GERMANY)
- Visiting Surgeon HELIOSENDO at klinik, Hamburg, Germany
Dr. Ashwani Maichand brings with him a rich experience of Orthopaedics, more than a decade of which has been dedicated to joint reconstruction.




