Avascular Necrosis of the Hip
Hip avascular necrosis is a dangerous ailment that has several potential causes. It is typified by excruciating pain and trouble walking. Many patients seek final treatment from an orthopedic surgeon after initially consulting with their primary care physician for pain management.
What is AVN Hip Replacement?
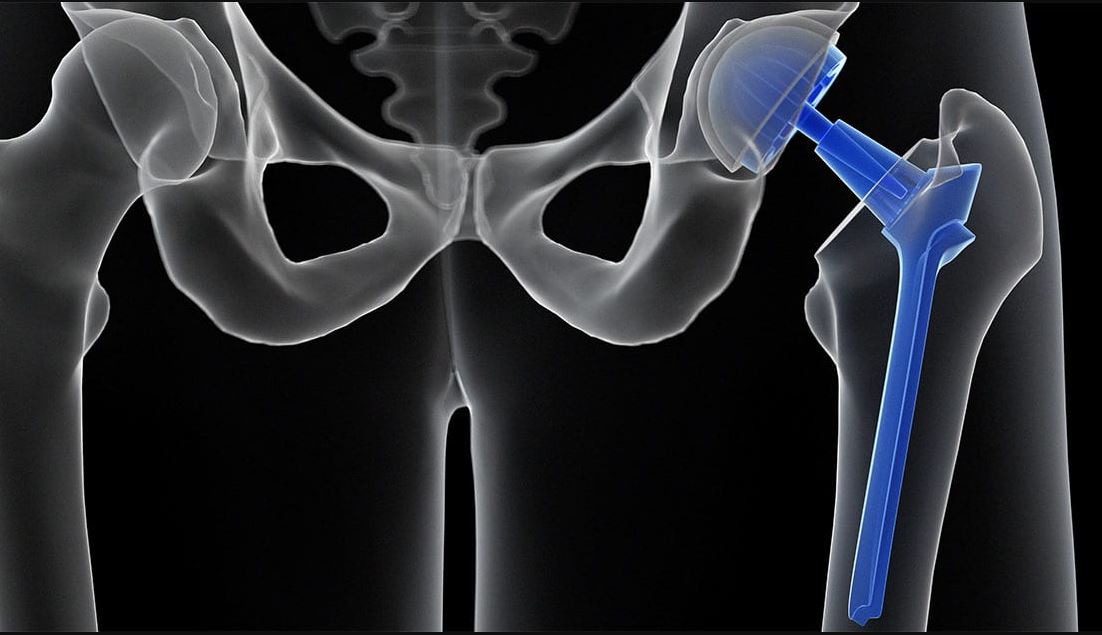
Most of the time, Avascular Necrosis (AVN) happens in the hip joint. Our hip is a ball and socket joint. In this disease, the blood supply to the ball is cut off because of certain reasons which are still unknown in 90% of the cases. The number one cause is steroid intake, the other causes are smoking and drinking alcohol and the solution is hip replacement.
Many young patients are misguided by some non-operating people that they can be cured by stem cells or by drilling, decompression techniques, or some medicines but this’s not true and the patients lose their time and money with these procedures.
How Is Hip Avascular Necrosis (AVN) Caused?
The hip is a joint where two bones meet. Specifically, the hip is where the head of the thigh bone, the femur, meets a specific part of the pelvis, the acetabulum. Avascular necrosis of the hip refers to the loss of blood supply to the femoral head. This insufficient blood supply to the bone causes the bone to become weak and eventually collapse, leading to pain and arthritis. The factors that cause this impaired blood flow vary.
Why Does AVN Occur?
Avascular necrosis has numerous causes, as previously mentioned. In actuality, the majority of scientists think that a confluence of circumstances functioning simultaneously to produce the ideal storm is what causes the illness. Both adults and children may experience this syndrome, which can be brought on by certain drugs, illnesses, or other circumstances.
Avascular necrosis is frequently caused by alcohol and glucocorticoids. Known by their common name, steroids, glucocorticoids are used to treat a wide range of illnesses. They may hinder blood flow to the femoral head in certain individuals, leading to bone deterioration. Avascular necrosis is also a result of excessive alcohol usage. Scientists think alterations in stress levels, a rise in fat, and slow blood flow are to blame for this.
Core decompression is a surgical procedure primarily used in the early stages of avascular necrosis (AVN) or osteonecrosis. This condition involves the loss of blood supply to a bone, often leading to bone tissue death. Core decompression aims to reduce pressure within the bone and stimulate new blood flow to the affected area, potentially preventing further bone collapse and the need for joint replacement surgery in the later stages of AVN.
However, it's essential to clarify that the success rate and effectiveness of core decompression surgery is 0%.
Conclusion
Hip avascular necrosis is a disorder that results in discomfort and decreased hip movement. The patient's lifestyle, risk factors, and other factors all influence the treatment plan, which is intricate. Make an appointment to consult with Dr. Ashwani Maichand if you have hip avascular necrosis so that you can decide on the best course of action.
Looking for Best AVN Specialist in Delhi? Contact Dr. Ashwani Maichand today.
Our Services

Dr. Ashwani Maichand
MBBS, MS(Orthopaedics) | Mch(Orthopaedics)
- Sr. Consultant & Director at Minomax Orthopaedics
- Director Orthopaedics, CK Birla Hospital
- Fellowship Joint Replacement (USA & GERMANY)
- Visiting Surgeon HELIOSENDO at klinik, Hamburg, Germany
Dr. Ashwani Maichand brings with him a rich experience of Orthopaedics, more than a decade of which has been dedicated to joint reconstruction.




